Nature’s Nanotechnology
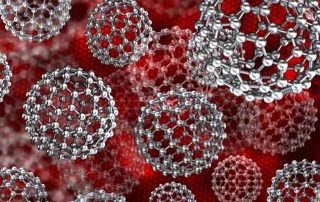
Nanotechnology is a revolutionary field of science and technology, with significant developments over the last few decades spanning medicine, cosmetics, agriculture, and engineering. The simple definition of ‘nano’ means particles sized 1 to 100 nm (1 billionth of a metre, not even visible with standard microscopy). They have a large surface area to volume, which can alter properties such as strength, dynamics, stability and reactivity – and it is this that makes them of huge scientific interest. It is often assumed that ‘nano’ always means ‘artificial’ or ‘engineered’. That’s not the case – nanoparticles are all around us in the natural world and have been for billions of years. Indeed, nature has been described as an ‘excellent nanotechnologist’.
In the atmosphere
 The land, sea and air are rich in examples of nanomaterials. In the atmosphere, nanoscopic ash or soot particles are present due to volcanic activity or near open fires, and dust storms from deserts contain many mineral-based nanoparticles. Mineral springs are full of nanoscopic solid material, and clay is a natural nanomaterial, made of silicon, aluminum and hydroxyl components forming sheets of nanometric size. These sheets give plasticity to the clay when wet, which then hardens upon drying or firing.
The land, sea and air are rich in examples of nanomaterials. In the atmosphere, nanoscopic ash or soot particles are present due to volcanic activity or near open fires, and dust storms from deserts contain many mineral-based nanoparticles. Mineral springs are full of nanoscopic solid material, and clay is a natural nanomaterial, made of silicon, aluminum and hydroxyl components forming sheets of nanometric size. These sheets give plasticity to the clay when wet, which then hardens upon drying or firing.
Nanotechnology is also an integral part of the living world. The living cell is microscopic in size (animal and plant cells are in the range of 0.01 – 0.10 mm, and bacteria are smaller), but many biological processes involve nanoparticles. A remarkable example is […]