Fungal Nail Infection (Onychomycosis) is the most common nail disorder.1 Risk factors such as trauma, old age, diabetes, immunosuppression, tinea pedis, psoriasis, and family history are leading to an increased prevalence.2
Onychomycosis is characterised by nail thickening, splitting, roughening and discolouration. Although viewed as ‘less serious’ than other infectious diseases, onychomycosis may cause significant disability, including pain, nerve damage, difficulties performing daily tasks, and has been linked to poor mental health and impaired social interactions.3
Onychomycosis is notoriously difficult to treat because the dermatophytes grow between the nail bed and plate but are protected by the nail.4 The efficacy of current treatments is limited by the slow growth of toenails, nail keratin thickness preventing penetration of topical and systemic drugs, and survival of fungi in surrounding environments (such as footwear) for long periods.5
Achieving a complete cure can take as long as eighteen months6 and may only be achieved at all in 20–25% of treated patients.7 While susceptibility to onychomycosis increases with the presence of other underlying disease, such as chronic renal failure and renal transplant, immunodeficiency, diabetes, cancer and peripheral arterial disease8,9 these comorbidities and associated treatments make some patients ineligible for oral antifungals. Systemic side effects associated with oral antifungals can lead to patient nonadherence and treatment failure. Furthermore, the incomplete clearance of fungal spores or hyphae can lead to recurrence in 40-70% of patients.10
Recent microbiological advances suggest that fungi, like bacteria, can form biofilms: complex microbial communities which permanently attach to epithelial surfaces in an extracellular matrix. The presence of a protective barrier created by fungal biofilms may partly explain the high rates of treatment failure, recurrence and relapse seen in onychomycosis.11
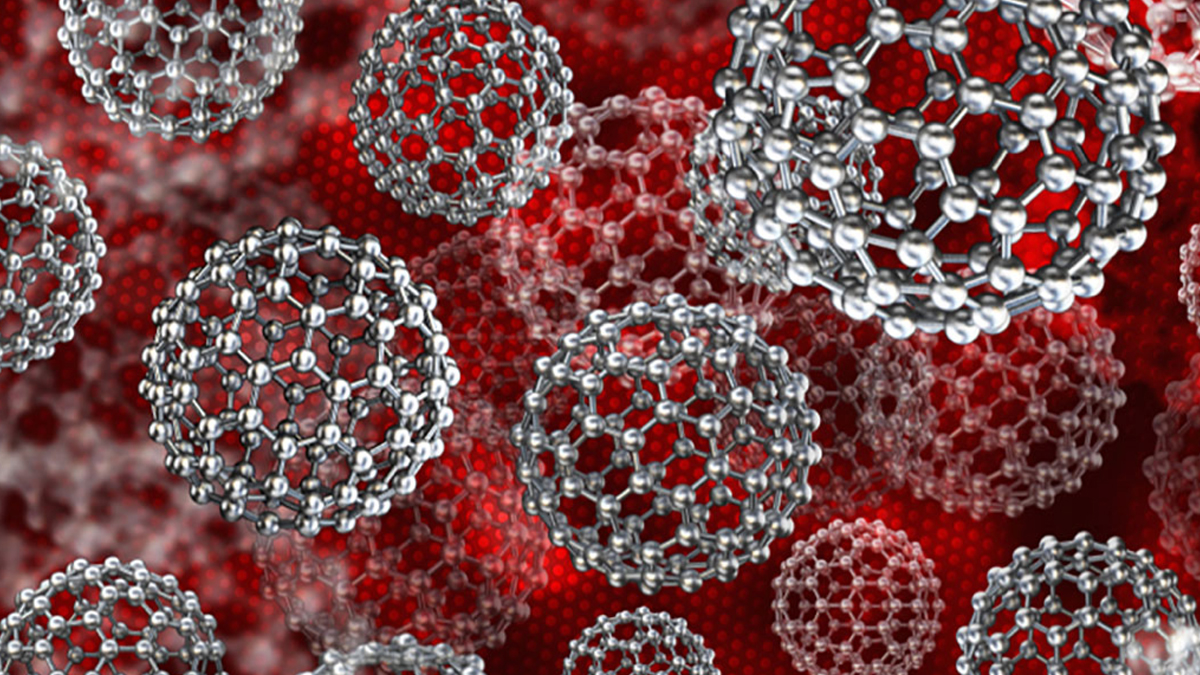
When developing a well-tolerated, topical antifungal there are challenges finding compounds that will penetrate the nail effectively without hindering the safety or efficacy of the drug.12 Researchers also face difficulty finding an optimal vehicle for topical use that will deliver effective drug levels to the site of the nailbed.13 Nanoparticles offer a solution, greatly enhancing cellular delivery of topical treatments with none of the safety concerns associated with systemic exposure in oral treatment.14 As such the development of new topical antifungals for onychomycosis has focused on topical formulations of current oral agents, new formulations of existing topical agents, and new chemical entities.15
Blueberry Therapeutics is developing a new topical nanomedicine, BB2603, for onychomycosis. The drug achieved its primary and secondary end points in our first Phase I/II clinical trial, so the company now plans to initiate a large phase II study for BB2603.
1 Lipner, S. R. Pharmacotherapy for onychomycosis: new and emerging treatments. Expert Opinion on Pharmacotherapy 2019, 1–11. doi:10.1080/14656566.2019.1571039
2 Gupta, A. K., & Mays, R. R. (2018). The Impact of Onychomycosis on Quality of Life: A Systematic Review of the Available Literature. Skin Appendage Disorders.doi:10.1159/000485632
3 Lipner SR, Scher RK. Onychomycosis: current and investigational therapies. Cutis. 2014;94(6):E21–24.
4 Elewski BE, Onychomycosis: Pathogenesis, Diagnosis and Management. Clin Microbiol Rev Jul 2018; 11 (3): 415-429 (Page 415)
5 Gupta, A.K.; Daigle, D.; Carviel, J.L. The role of biofilms in onychomycosis. J. Am. Acad. Dermatol. 2016, 74, 1241–1246.
6 Scher, R.K.; Baran, R. Onychomycosis in clinical practice: Factors contributing to recurrence. Br. J. Dermatol 2003, 149, 5–9.
7 Elewski, B.E.; Tosti, A. Risk factors and comorbidities for onychomycosis: Implications for treatment with topical therapy. J. Clin. Aesthet. Dermatol. 2015, 8, 38–42.
8 Ghannoum, M.; Salem, I.; Christensen, L. Epidemiology of onychomycosis. In Onychomycosis; Rigopoulos, D., Elewski, B., Richert, B., Eds.; JohnWiley & Sons: Hoboken, NJ, USA, 2018.
9,11,12,15 Tosti, A.; Elewski, B.E. Onychomycosis: Practical approaches to minimize relapse and recurrence. Skin Appendage Disord. 2016, 2, 83–87.
10 Thomas J (2010) Toenail onychomycosis: an important global disease burden; J Clin Pharm and Therapeutics 35, 497–519 (Page 503)
13 Del Rosso, J.Q. The Role of Topical Antifungal Therapy for Onychomycosis and the Emergence of Newer Agents; J Clin Aesthet Dermatol. 2014 Jul; 7(7): 10–18 accessed online 1/3 via: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4106353/
14 Zheng Zhang,a Pei-Chin Tsai,b,c Tannaz Ramezanli,b,c and Bozena B. Michniak-Kohna,b,c,, Polymeric nanoparticles-based topical delivery systems for the treatment of dermatological diseases; Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2013 May; 5(3): 205–218 accessed online via https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3631287/